Key Takeaways
- Berkeley Lab researchers and their Harvard collaborators examined cell type and brain region specific features of DNA repair in normal brains in a first-of-its-kind study.
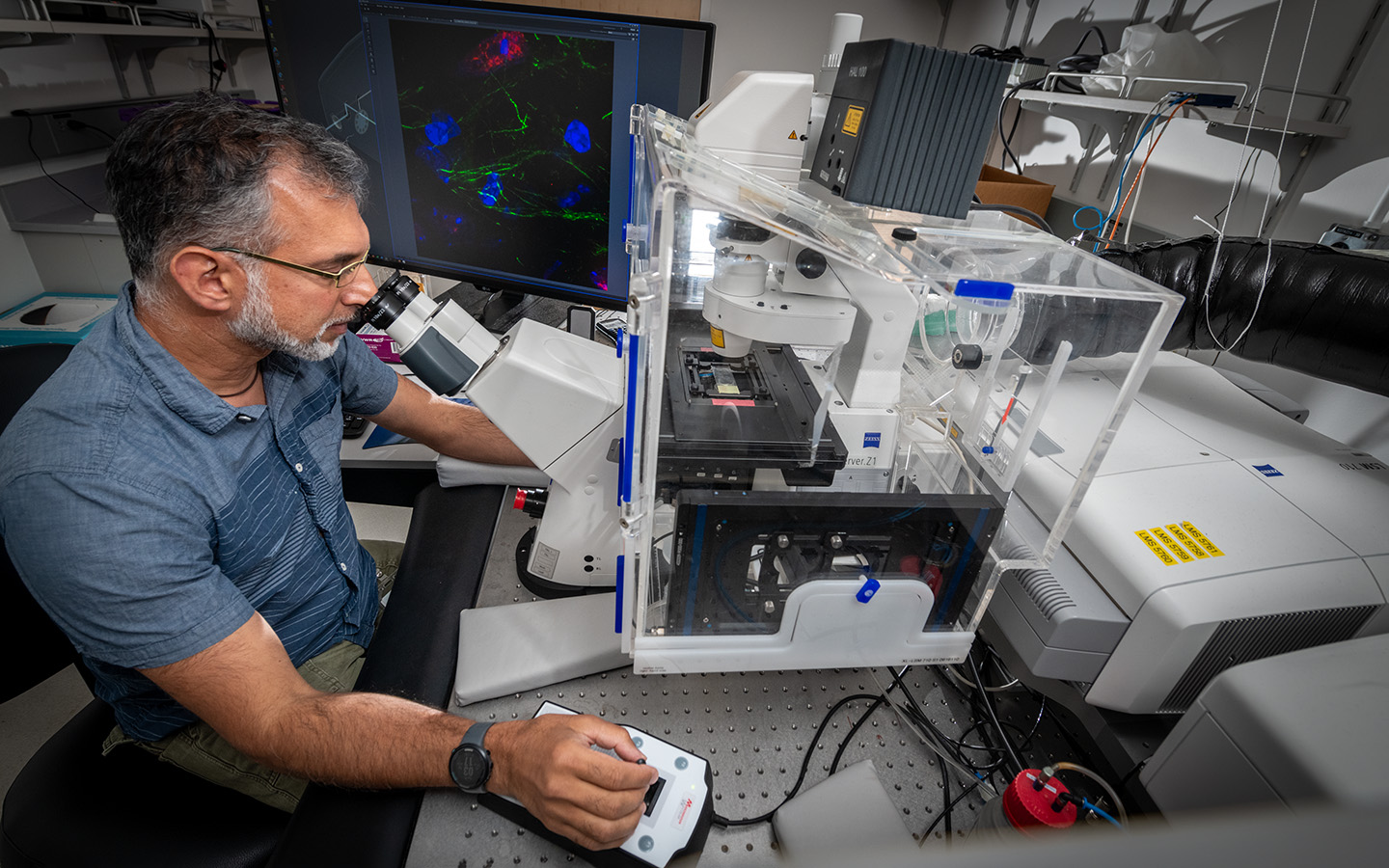
- The team employed advanced immunofluorescence capabilities available at Berkeley Lab to image neural cells in intact brains.
- The results provide insight into the role of DNA repair in healthy aging and neurodegenerative disease progression.
Brain cells receive sensory inputs from the outside world and send signals throughout the body telling organs and muscles what to do. Although neurons comprise only 10% of brain cells, their functional and genomic integrity must be maintained over a lifetime. Most dividing cells in the body have well-defined checkpoint mechanisms to sense and correct DNA damage during DNA replication.
Neurons, however, do not divide. For this reason, they are at greater risk of accumulating damage and must develop alternative repair pathways to avoid dysfunction. Scientists do not understand how neuronal DNA damage is controlled in the absence of replication checkpoints.
A recent study led by Cynthia McMurray and Aris Polyzos in Lawrence Berkeley National Laboratory's (Berkeley Lab's) Molecular Biophysics and Integrated Bioimaging Division addressed this knowledge gap, shedding light on how DNA damage and repair occur in the brain. Their results suggest that DNA damage itself serves as the checkpoint, limiting the accumulation of genomic errors in cells during natural aging. The paper, published in Nature Communications, offers clues to understanding the potential role of unrepaired DNA damage in the progression of neurodegenerative diseases and could help inform the development of therapies.
The brain is highly specialized, with neurons in different regions performing distinct cognitive and motor roles, and, depending on their function, neurons vary in their energy requirements. As the first study to integrate cell type- and brain region-specific features of DNA repair in normal brains, this work sets a benchmark for the field
"When we started this work there had not been a study that looked in-depth at the regional component of DNA damage in the brain," said Polyzos, a research scientist and first author on the paper. "Since many of the internal DNA damaging agents in neural cells arise from energy production, and since metabolic activity varies throughout the brain, we suspected that there would also be regional variation in DNA damage and its regulation."
In collaboration with Zachary Nagel's lab at the T.H. Chan School of Public Health at Harvard University, the Berkeley Lab researchers employed a bevy of innovative techniques to measure the DNA repair capacity, repair protein expression profiles, and double-strand break levels across brain regions in healthy mice. First, the researchers confirmed the presence of major DNA repair pathway machinery in each of four brain regions: the cerebral cortex, the hippocampus, the cerebellum, and the striatum.
Members of Nagel's group then determined the capacities of the various DNA repair pathways in the different brain regions using a technique called "fluorescence multiplex host cell reactivation" developed in their lab. In addition, the team at Berkeley Lab imaged neural cells in intact brains using immunofluorescence techniques, allowing distinction between the various cell types in the brain and maintaining a physiological context for DNA damage and repair.
"Since many of the internal DNA damaging agents in neural cells arise from energy production, and since metabolic activity varies throughout the brain, we suspected that there would also be regional variation in DNA damage and its regulation."
– Aris Polyzos
Single-strand breaks generated during DNA repair were observed converting to double-strand breaks and reversibly switching between states in response to oxidation in cultured neurons as well as in living mouse brains. The cell uses the reversible interconversion as a physiological checkpoint to both produce unrepaired double-strand breaks for productive functions, but also restricts them from exceeding tolerable limits. Although oxidative damage originates as part of normal metabolism, the researchers found that high levels of oxidative damage can lead to aging and disease if the accumulation of breaks increases beyond a normal threshold.
"The paper is a nice study of the steady-state level of DNA breakage in brain and supports the long-held view that oxidative stress is a source of such breakage-including the conversion of single-strand breaks to double-strand breaks," observed Keith Caldecott, co-director of the Genome Damage and Stability Centre at the University of Sussex and an expert in the field of DNA damage, who did not contribute to the paper. "The hypothesis that such breaks themselves are a regulatory signal, rather than simply an obligate intermediate of a regulatory reaction, is intriguing and provocative."
Moreover, the study provides a more thorough basis to interrogate DNA damage and repair observed during the progression of neurodegenerative diseases including Alzheimer's, Huntington's, and Parkinson's. McMurray, Polyzos, and their team have been studying dysregulation of energy production in neurons in Huntington's disease and are currently investigating DNA damage seen in these neurons during disease progression. Evidence of a pathway between energy dysregulation and neurodegeneration could ultimately provide a therapeutic target for Huntington's disease.
"It's critical to know the source of genome instability that arises from within cells and underpins the many DNA repair-defective syndromes characterized by neurodegeneration or abnormal neurodevelopment," noted Peter McKinnon, vice-chair of the Department of Cell & Molecular Biology at St. Jude Children's Research hospital and another expert in the field, specifically with respect to DNA damage caused by disease. "In this new report, the investigators show the conversion of single-strand breaks to double-strand breaks via oxidative damage is a key event in generating detrimental types of genome damage. This is an important finding and helps us understand how these neurological diseases arise."
This work was supported by the National Institutes of Health.






