Breast cancer is becoming increasingly treatable, but in some cases the disease can resurface even decades after a patient has been declared cancer free. This is because of cells that detach from the original tumor and hide in a dormant state in the breast or other organs. Little is known about the mechanisms responsible for dormancy in cancer cells, and even less is known about what causes these cells to suddenly wake up. A new study from the laboratory of Israel Prize laureate Prof. Yosef Yarden at the Weizmann Institute of Science, being published today in Science Signaling, reveals the mechanism that puts breast cancer cells to sleep, as well as the reason that they emerge from dormancy more aggressive than they were before they became dormant.

From the earliest stage of embryonic development, through sexual maturation to the production of breast milk during pregnancy and after childbirth, breast tissue changes throughout a woman's life. These changes are made possible by the metamorphosis that breast tissue cells undergo, from the early developmental stage, known as mesenchymal, when the cells are round, highly mobile and dividing rapidly, to the more mature, epithelial stage, when they are somewhat cubical, less active and dividing slowly. The cells move back and forth between these stages in a controlled and gradual process, but sometimes they go out of control, dividing rapidly and becoming malignant. This cancer process begins when mature cells return to their earlier, developmental stage, which allows them to divide rapidly, create tumor tissue and even migrate to other tissues. Later on, however, the cancer can benefit from exactly the opposite process: Cells that have spread throughout the body can revert to their mature state, becoming immobile and slow. Essentially, they become dormant.
""The common belief is that dormant cancer cells exist in a suspended state, but we have shown that they accumulate DNA mutations"
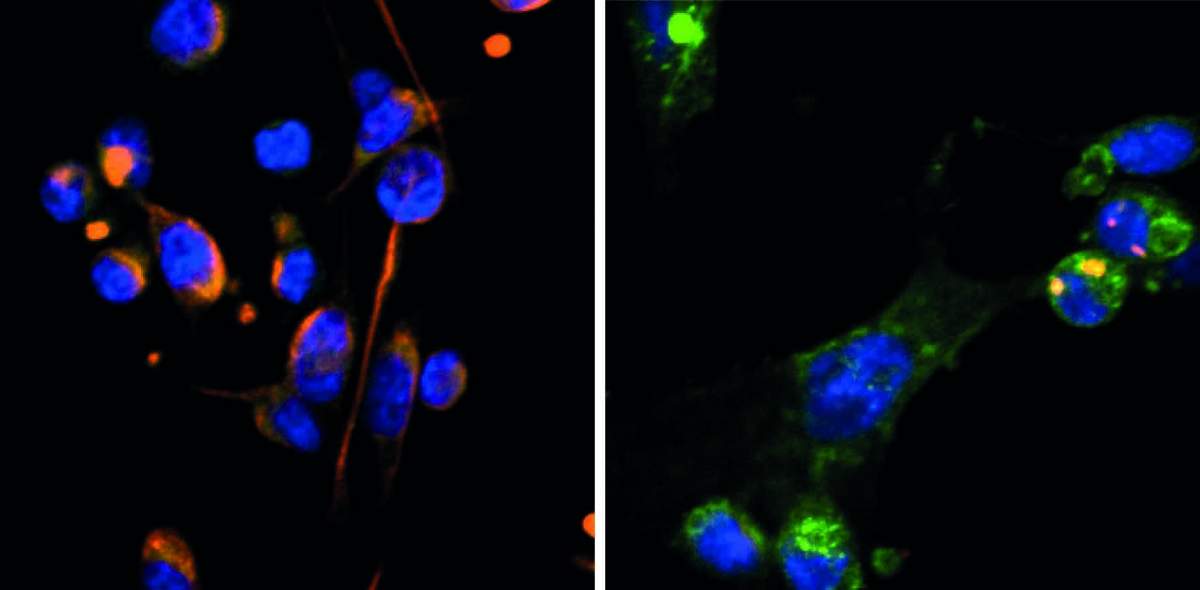
Because of the major similarities between entry into dormancy and the maturation process of epithelial cells, scientists in Yarden's lab in Weizmann's Immunology and Regenerative Biology Department postulated that they might be able to induce a state of dormancy in breast cancer cells by imitating the natural process. Using a three-dimensional model of a cancerous tumor environment developed by Dr. Dalit Barkan of Haifa University, the researchers, led by Dr. Diana Drago-Garcia from Yarden's team, genetically modified human breast cancer cells of the most aggressive type, called triple-negative breast cancer, to produce higher levels of OVOL proteins, which are known to be involved in the natural maturation of epithelial cells. The model showed that increasing the expression of two OVOL proteins halts the lifecycle of aggressive cancer cells and induces dormancy. In parallel, the researchers showed, in female mice implanted with human tumor tissue, that over-expression of OVOL inhibits the growth of the cancer.
Although halting the lifecycle of cancer cells and slowing tumor growth might sound like good news and perhaps even the basis for a future treatment, it is known that cancer patients' breast tissue contains elevated levels of one of the OVOL proteins. The scientists therefore hypothesized that while this protein, OVOL1, slows cancer in the short term, it is beneficial to cancerous cells in the long term, enabling them to enter a state of dormancy and survive for years without being detected. When conditions in the body change and the level of OVOL1 drops, the cancer comes back to life and is more aggressive than ever before.
Armed with these findings, the researchers began to study how the cancer affects the expression levels of OVOL proteins, putting tumor cells to sleep or waking them up. One key finding was that certain growth factors boost OVOL1 expression, but the steroid hormone estrogen suppresses it. The scientists went on to show that patients with low levels of estrogen receptors and high levels of OVOL1 tend to develop more aggressive cancer and have lower chances of survival.
"These findings could pave the way for preventing cancer cells from going dormant or stopping dormant cells from reawakening," Yarden says. "We know, for example, that fat tissue takes control of estrogen production during menopause. So, we can assume that weight gain in older women who had cancer when they were younger could increase the risk of dormant cancer resurfacing because of increased estrogen production and the associated drop in OVOL1 expression. In the future, these hypotheses can be tested in animal models and in human patients."
Changing in their sleep
One of the questions that remained unanswered was why breast cancer tends to be more aggressive when it awakens from a state of dormancy. To uncover the underlying mechanisms, the researchers traced the molecular signaling pathway through which OVOL1 induces dormancy. They discovered that this pathway triggers an accumulation of unstable molecules known as free radicals, which leads to widespread cellular damage, cell cycle arrest and dormancy. This build-up was surprising, since these molecules had not previously been linked to dormancy in cancer cells.

Later, the researchers, working with Prof. Emeritus Yosef Shiloh of Tel Aviv University, showed that the continuous cellular stress within the dormant cells, resulting from the accumulation of the free radicals, changes the expression and function of proteins in the cells' nuclei, which house their genetic material. Consequently, the genetic material is oxidized and its integrity is compromised, as is the functioning of three key proteins involved in DNA repair mechanisms. The scientists believe that the widespread damage to the genetic material and the failure of the repair mechanisms explain why, when a cancer cell awakens, it carries numerous mutations, making it more aggressive and resistant to treatment.
"The common belief is that dormant cancer cells exist in a suspended state, but we have shown that during their so-called sleep they accumulate DNA mutations because of the oxidative process, and they undergo a major change," Yarden explains. "This discovery is consistent with the analysis of tissue samples from aggressive breast cancer tumors. Importantly, breast cancer is not the only malignancy that enters a state of dormancy, so understanding the mechanisms of dormancy could lead to new treatments for various other types of cancer, as well."
Science Numbers
Some 40 percent of patients with stages 1 to 3 triple-negative breast cancer experience a recurrence after standard treatment.
Also participating in the study were Dr. Suvendu Giri, Dr. Rishita Chatterjee, Dr. Arturo Simoni-Nieves, Dr. Maha Abedrabbo, Dr. Alessandro Genna, Dr. Mary Luz Uribe Rios, Dr. Moshit Lindzen, Dr. Arunachalam Sekar, Nitin Gupta, Noa Aharoni, Tithi Bhandari, Agalyan Mayalagu, Feride Karatekin, Yam Nof, Dr. Nishanth Belugali Nataraj, Prof. Ronen Alon and Prof. Rony Seger from Weizmann's Immunology and Regenerative Biology Department; Luisa Schwarzmüller, Dr. Nooraldeen Tarade and Prof. Stefan Wiemann from the German Cancer Research Center (DKFZ), Heidelberg; Dr. Rong Zhu, Dr. Yaniv Eyal-Lubling, Prof. Oscar Rueda and Prof. Carlos Caldas from the University of Cambridge; Dr. Harsha-Raj Mohan-Raju and Prof. Sima Lev from Weizmann's Molecular Cell Biology Department; Dr. Francesco Roncato from Weizmann's Molecular Genetics Department; Dr. Tal Keidar and Prof. Eli Pikarsky from the Hebrew University Hadassah Medical School, Jerusalem; Karin Shira Bernshtein from the University of Haifa; Dr. Bettina Wagner and Prof. Maik Dahlhoff from the University of Veterinary Medicine Vienna; Dr. Nishanth Ulhas Nair, Neel Sanghvi and Prof. Eytan Ruppin from the National Institutes of Health, Bethesda, USA; Dr. Sara Donzelli and Prof. Giovanni Blandino from the IRCCS Regina Elena National Cancer Institute, Rome; and Prof. Ron Prywes from Columbia University, New York.
Prof. Yosef Yarden is head of the Dwek Institute for Cancer Therapy Research and the incumbent of the Harold and Zelda Goldenberg Professorial Chair in Molecular Cell Biology.






