Did you know that shellfish allergy is very common in adults and children? In fact, shellfish is the leading cause of food allergy in the U.S. It affects around 3% of adults and a little over 1% of children.
People with a shellfish allergy can react to one or more foods in the shellfish family, including shrimp, crab, lobster, clam, oyster and mussels. The allergy can induce a strong immune response. Patients with shellfish allergy can develop mouth and throat itching, lip swelling and skin reactions, such as hives, puffy eyes and skin redness.
In some people, an allergic reaction to shellfish can be severe and life-threatening – called anaphylaxis. Symptoms may include vomiting, dizziness or fainting and trouble breathing due to constricted airways. In rare cases, without immediate treatment with epinephrine, it can lead to death.
Despite its prevalence and its potentially lethal symptoms, shellfish allergy remains a big challenge to clinicians to diagnose and treat.
In their review published in Current Opinion in Allergy and Clinical Immunology, Patrick Leung and Christine Wai examined the current status in the diagnosis and clinical management of shellfish allergy. They highlight the imminent need for more specific diagnostic methods and effective and safe therapeutic approaches for shellfish allergy.
In this Q& A, Leung who is a professor of rheumatology, allergy and clinical immunology at UC Davis Health, answered questions on the latest advances in diagnosing and treating shellfish allergies.
Let's start with the basics. What causes shellfish allergies?
Food allergies in general result from an immune system overreaction. The immune system defends the body from invaders, such as infections. A food allergy occurs when the body identifies a food substance (known as an allergen) as a foreign invader in genetically susceptible individuals. This leads to an army of immune players orchestrating a series of reactions aiming at removing the invader. These reactions are manifested as allergy.
There are many known allergens that might cause shellfish allergy. In fact, our review identified 49 crustacean allergens and eight in the mollusk family. However, among all allergens, tropomyosin is best recognized as the major allergen and the most well studied shellfish allergen. It is also common in arthropods, like house dust mites and cockroach.
What are the standard diagnostic tests for shellfish allergy?
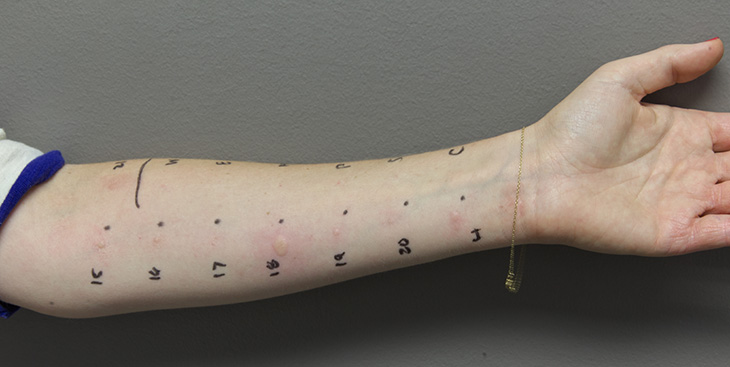
To diagnose shellfish allergy, the routine workup would involve a thorough review of the patient's history, a skin prick test, and a blood test for shellfish allergens and tropomyosin. Clinicians would then assess whether an oral food challenge is necessary to confirm a diagnosis.
Still, these tests might not be conclusive.
A blind food challenge remains the gold standard for food allergy diagnosis. However, this method is resource-intensive, time-consuming, expensive and with the risk of severe reaction that hampers its clinical use. Food challenges are held in a medical facility. The patient is given a small amount of the food to eat and watched carefully for any reactions. Over the course of several hours, they will slowly consume larger and larger amounts of the food while under medical supervision to determine whether they are allergic
Recently, there has been a successful study on using nasal allergen provocation test to diagnose shellfish allergy. Yet, there is still a great need for a noninvasive but accurate diagnostic method for shellfish allergy.
Based on your review, what would the best diagnosis plan look like?
It is known that skin prick tests and blood antibody tests have low specificity. So, for patients with a history of shellfish allergy and negative skin and blood tests, we can do component-resolved diagnosis (CRD) and antibody crosslinking tests to test for allergen specific IgE in blood samples. These diagnostic strategies are to determine the diagnosis of shellfish allergy. Food challenges are offered only when the results are uncertain to minimize risks to the patient.
How long does it take shellfish allergy to resolve, if at all? Do people outgrow their shellfish allergy?
Most people do not outgrow shellfish allergies. Studies show that 46% of people allergic to shrimp outgrew their shrimp allergy in 10 years. Meanwhile, patients are advised to avoid shellfish in their diet and take rescue medication — epinephrine — in case of an allergic episode.
What role does immunotherapy play in treating allergies?
Immunotherapies are designed to desensitize food-allergic patients and to restore food tolerance in order to improve the quality of life of patients. Although there are many experimental immunotherapy approaches for shellfish allergy, we still need clinical studies with large cohort of shellfish allergic subjects to rule on the efficacies of these treatments. It is our hope that effective allergen specific immunotherapy will improve the quality of life in affected individuals.
What do we know about the use of herbal medicines and probiotics in regulating allergic reactions, especially shellfish allergies?
One emerging immunotherapy approach is the use of traditional Chinese herbal medicine, such as the FDA-approved herbal formulation FAHF-2. Clinical trials showed that FAHF-2 treatment was safe and well-tolerated but with limited efficacy.
As for probiotics, they are commonly consumed as dietary supplements. They have been shown to modulate the immune system in allergic populations. Lactobacillus and Bifidobacterium are the two main probiotics shown to protect against atopic disease. Recent preclinical studies highlight the potential of probiotic supplementation to restore oral tolerance against shrimp allergy. A combination of probiotics and oral immunotherapy may be a possible strategy to enhance the safety and efficacy of allergen-specific immunotherapy.
What are some of the potential treatments for an allergic reaction?
Anti-inflammatory drugs (such as corticosteroids) and anti-IgE (like omalizumab) are mainstream nonspecific treatments that can be used alone or used in combination with oral immunotherapy for rapid desensitization and to reduce risk of allergic reactions. Other treatment options prescribed according to the needs of the patients include antihistamines and epinephrine.






